How Daily Diet Affects Crohn is Disease: The Immortal Cancer
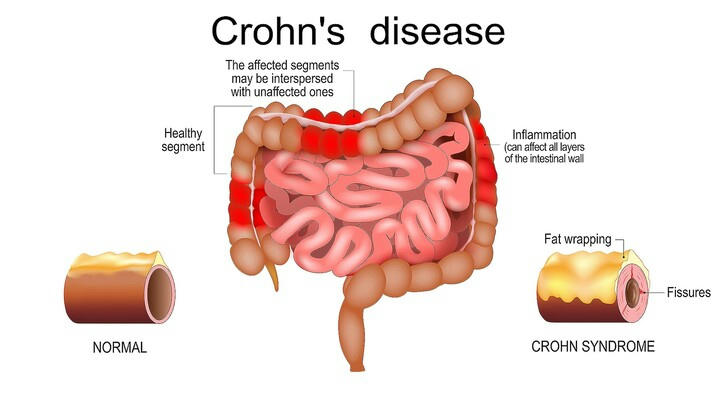
Crohn’s disease, often dubbed the “immortal cancer,” is a chronic inflammatory condition of the gastrointestinal tract. Unlike cancer, Crohn's disease is not malignant, but its continuous and often unpredictable flare-ups can make it feel relentless and incurable.
Managing this condition involves more than just medication; diet plays a crucial role in influencing both the severity and frequency of flare-ups. Certain foods can increase inflammation or trigger flare-ups, while others may help reduce symptoms. It’s important to note that dietary management isn’t a one-size-fits-all solution; instead, it requires a personalized strategy based on individual triggers and nutritional needs.

Fiber Intake: A Double-Edged Sword
Fiber is often a contentious topic for Crohn’s patients. While dietary fiber is generally considered beneficial for digestive health, in the case of Crohn’s disease, it can sometimes worsen symptoms. High-fiber foods, such as whole grains, nuts, and raw vegetables, can irritate the inflamed gut lining, leading to increased abdominal pain and diarrhea.
During flare-ups, many patients are advised to follow a low-fiber diet to minimize irritation and promote healing. However, in periods of remission, incorporating soluble fiber from sources like oatmeal and bananas might be beneficial, as it can help with stool consistency and overall gut health.
Fats and Their Role in Managing Crohn’s
High-fat diets can exacerbate symptoms for some individuals, particularly those with Crohn’s affecting the small intestine. Fatty foods can lead to malabsorption issues, where essential nutrients are not properly absorbed, leading to deficiencies.
On the other hand, omega-3 fatty acids, found in fish oil and flaxseeds, have anti-inflammatory properties. Many studies have shown that omega-3 fatty acids may help relieve inflammation in Crohn's disease by reducing levels of inflammatory mediators, such as interleukins and tumor necrosis factor. It can reduce the frequency of abdominal pain and diarrhea in patients, thereby improving quality of life.
Some studies have also found that omega-3 fatty acids may help prolong remission and reduce the frequency of disease relapses, but the results are not always consistent. Therefore, omega-3 fatty acids are generally considered as part of a comprehensive treatment rather than a single treatment because of individual differences.

Proteins and Nutritional Balance
Protein intake is vital for maintaining muscle mass and overall health, particularly for those experiencing weight loss due to Crohn’s.Patients can choose proteins with high biological value, such as eggs, whey protein, fish and other proteins with high digestibility and absorption, and pay attention to avoid cooking methods such as frying and heavy seasoning. Plant proteins and low-fat, low-fiber proteins, such as tofu and soy milk, chicken, turkey and other lean meats can also be considered.
At the same time, patients should be cautious about consuming protein sources that are difficult to digest,such as red meat or processed proteins, which may exacerbate symptoms. Balanced protein consumption, alongside other nutrients, supports the body in managing inflammation and repairing tissues, especially during periods of remission.

Carbohydrates and Gut Health
Simple carbohydrates, found in sugary foods and beverages, can exacerbate inflammation and contribute to diarrhea. Conversely, complex carbohydrates from sources like sweet potatoes and brown rice, when tolerated, provide essential nutrients and energy without causing undue irritation. It is essential for individuals with Crohn’s to monitor their carbohydrate intake and opt for easily digestible sources to maintain stable blood sugar levels and prevent symptoms.
Hydration and Electrolyte Balance
Proper hydration is crucial for managing Crohn’s disease, particularly for those who experience frequent diarrhea. Dehydration can exacerbate fatigue and exacerbate the overall impact of the disease. Electrolyte-rich beverages and broths can help replenish lost nutrients and maintain fluid balance. Avoiding caffeinated and alcoholic drinks, which can irritate the gut, is also recommended.
One man who achieved success with the exclusive enteral nutrition (EEN) program had moderate to severe Crohn's disease, and his daily life was severely impacted by persistent abdominal pain, frequent diarrhea, and weight loss. On his doctor's recommendation, he began an 8-week exclusive enteral nutrition (EEN) program.
This program involves consuming only a liquid diet consisting of medically formulated nutritional shakes or formulas, and nothing else, designed to provide all the necessary vitamins, minerals, proteins, carbohydrates, and fats without the potential irritants found in solid foods. Over time, the patient's abdominal pain was significantly reduced, his diarrhea became less frequent, he gained weight, and ultimately his intestinal inflammation improved.

Summary
In conclusion, daily dietary choices play a significant role in the management of Crohn’s disease. While there is no one-size-fits-all approach, careful attention to fiber, fats, proteins, carbohydrates, and hydration can help mitigate symptoms and improve quality of life. As research continues to evolve, a personalized dietary approach, guided by medical professionals, will remain crucial for those navigating the complexities of this chronic condition.
